Ambulance service in Texas now delivering home care

For more than a decade, John Farris traveled through the streets of Fort Worth, Texas, working 911 calls. As a paramedic for MedStar, he would ask himself: Could he prevent these 911 calls in the first place?
It’s a question that went against the very business model of MedStar until recently — a question most emergency medical services companies don’t talk about, because the more trips to the hospital, the more money the company makes. But it still mattered to Farris. So, sometimes, after stabilizing a patient in the back of the ambulance, he’d try to squeeze in a conversation about nutrition or hydration.
“I’d be lucky if I got 10 minutes to talk with them,” he said.
Now, he gets a full hour with five patients each day.
Traditionally, ambulance crews arrive with sirens blaring, ready to rush someone to the hospital. In Fort Worth, some paramedics are doing the opposite: scheduling visits to treat patients in their homes. This idea — what’s called mobile integrated health care — is gaining traction as a way for hospitals to save money.
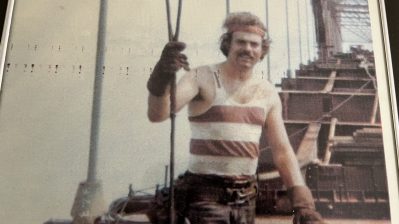
Farris still works for MedStar. He still carries a bag with a CPR kit and gauze and gloves, but he rides in a four-door sedan, not an ambulance. Farris is what’s called a community paramedic. It’s his job to see the trickiest patients, the so-called “frequent flyers” who keep landing back in the emergency room. Since the Affordable Care Act, the government penalizes hospitals for re-admissions. So these patients are costing hospitals across the country hundreds of millions of dollars. Farris is trying to figure out why they keep returning.
Today’s second stop is at Sandra Guevara’s apartment in Fort Worth. It’s dark, and the black curtains are closed. Guevara, who is in her early 30s, sits on her couch wrapped in a Dallas Cowboys blanket while she gets her blood pressure taken.
Last year, Guevara went to the emergency department more than 20 times, occasionally needing a ventilator to breathe.
“My asthma has been going on since I was 14 years old,” she said. “My anxiety triggers it when I go places, so I tend to shelter myself and stay home all the time.”
Guevara is on Medicaid, so she generally doesn’t have to pay the more than $1,000 each visit might cost. But those visits are something the government, hospitals and especially Guevara want to avoid.

Sandra Guevara talks with John Farris, a community paramedic who works for MedStar in Fort Worth, Texas.
“I don’t like going to the ER,” she said. “Especially when they put me in a little bitty room. I’ll start crying and shaking and everything. I can’t deal with it.”
Farris said from the perspective of the doctor in the emergency room, patients like Guevara can be labeled noncompliant. They’re sometimes seen as patients who won’t follow medical orders. But he said if you spend time getting to understand the situation, that’s not usually the case.
“The mental health needs that [Guevara] has, tied in with her asthma, tied in with her allergic asthma, tied in with her clotting factor, all of this stuff together, even her dehydration, all of it together is combining factors to make her worse. And every time she was out of the hospital she was back in a couple of days,” Farris said.
He’s helped Guevara modify her diet, convinced her to drink more water and consistently take her medication. He also made sure her doctors know what’s going on and connected her to a psychiatrist. Next visit, they plan to tackle one of her fears and take a short walk outside.
Taking walks with patients, talking to them about their fears, setting up social services like Meals on Wheels, is a major shift in emergency medicine.
When MedStar started enrolling patients for its mobile integrated health care program in 2009, it was one of the first in the country. Today, there are more than 260 similar programs.
Dr. Darrin D’Agostino, associate dean of community medicine at UNT Health Science Center, said early studies show pairing frequent hospital users with community paramedics can save money by preventing re-admissions in the long run.
“Some programs are actually showing decreases of 80 to 90 percent re-admission because the services that are needed are things that are not necessary provided by the physician,” D’Agostino said.
That includes things like making sure a patient has the right medicine — and calling the electricity provider to pay a bill and keep the lights on.
MedStar reports saving $17,000 per patient over a three-year period. The challenge, D’Agostino said, is securing initial funding. Right now, most emergency services are paid for ferrying patients to the hospital.
Since MedStar’s community paramedicine program is paid for by hospitals and health providers trying to save costs, it’s not clear if it would be affected by changes to the Affordable Care Act. The company is counting on a continued focus on the quality of care — and cost-cutting — no matter what happens with the ACA. It just helped publish a textbook on how to provide home care that’s now available nationwide.
There’s a lot happening in the world. Through it all, Marketplace is here for you.
You rely on Marketplace to break down the world’s events and tell you how it affects you in a fact-based, approachable way. We rely on your financial support to keep making that possible.
Your donation today powers the independent journalism that you rely on. For just $5/month, you can help sustain Marketplace so we can keep reporting on the things that matter to you.